Skin Cancer
What Is Basal Cell Skin Cancer?
Basal cell skincancer is by far the most common form of skin cancer in the United States. It is believed to occur when ultraviolet radiation (usually sunlight) damages the genetic material of the basal cells located in the thin, top layer of the skin (epidermis) or hair follicles.
The most common site for basal cell skin cancer is the face (typically the nose or ears), although it may appear anywhere. It is usually a painless, slow-growing cancer and very rarely, if ever, spreads to other parts of the body. Left untreated, however, it can slowly invade and even destroy the entire nose or an ear. Fortunately, with early detection and treatment, basal cell carcinoma is cured in 95% of cases, with only 5% of cases showing local recurrence.
Who Gets Basal Cell Skin Cancer?
皮肤癌是最常见的癌症,和basal cell carcinoma is the most prevalent type of skin cancer, striking one out of every eight Americans, including people in their 20s and 30s, women as well as men. It represents about one-third of all newly diagnosed cancers in the United States.
The most common site for basal cell carcinoma is the face, especially the nose or ears, but it can appear on any sun-exposed areas of skin. It is usually painless and slow growing, and rarely spreads to other parts of the body.
Symptoms
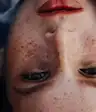
A small, flat, waxy or pearly bump, most common on the face, ears, back, or the “V” where the neck meets the chest.
A skin sore that doesn’t heal and that may crust, bleed, or ooze.
A sore or bump indented (sunken) in the middle.
A skin blemish that grows steadily over a period of weeks and does not spontaneously disappear within a month. It may develop into a shallow ulcer with raised edges and a moist center. The ulcer may seem to heal or disappear, only to recur later.
Causes/Risk Factors
Skin cells are damaged by cumulative exposure to ultraviolet radiation from the sun or from artificial sources (such as sunlamps). Although the risk of skin cancer increases steadily with age, even teenagers with excess sun exposure can develop skin cancers.
People who sunburn easily, especially those with fair skin, blue eyes, or red or blond hair are most at risk, because they have relatively little natural pigment protection (melanin).
Risk is greater in year-round sunny climates, where the sun’s radiation is most constant and intense.
In comparison to women, men have a two-fold higher risk of developing basal cell carcinoma.
There are some genetic diseases in which a person is predisposed to getting multiple basal cell carcinomas.
What If You Do Nothing?
If untreated, all forms of skin cancer will ultimately become destructive. Basal cell carcinomas are slow growing, but it is important that they be found and treated early because they can ultimately invade and destroy nearby tissues. More aggressive forms of basal cell carcinoma can spread to other parts of the body or become disfiguring.
Diagnosis
A physician can often diagnose basal cell carcinoma on sight; however, definitive diagnosis is essential, especially given the possibility of morpheaform BCC (a form of basal cell carcinoma that may look like a scar and can blend in with the surrounding skin, thus escaping detection for years while continuing to spread).
A skin biopsy (removal of a tissue sample for examination by a pathologist) is performed to confirm the diagnosis and to guide treatment options. A biopsy also may be used to rule out a more aggressive form of skin cancer (e.g., malignant melanoma).
Treatment
Treatment for basal cell carcinoma depends on the stage of the disease (i.e., whether it has spread to surrounding tissue), the size and location of the tumor, and the patient's overall health. Standard treatment may include surgery, radiation therapy, and chemotherapy. In some cases, more than one treatment is used. But when caught in time, basal cell carcinoma can often be removed by a doctor on an outpatient basis.
Types of surgeryinclude the following:
Cryosurgery or cryotherapy (an instrument is used to freeze and destroy cancer cells).
Curettage and electrodessication (a sharp instrument[curette]is used to remove cancer cells and then electric current is applied to control bleeding and destroy remaining cancer cells).
Dermabrasion (a rotating instrument is used to remove cancer cells).
Laser surgery (a laser is used to remove cancer cells).
Mohs micrographic surgery (often used to treat skin cancer on the face because it removes little normal tissue; the lesion is removed in layers and each layer is examined under a microscope for cancer cells).
Shave excision (cancer cells are shaved off the skin surface).
Simple excision (cancer cells and surrounding normal tissue is removed).
Radiation therapyuses high-energy x-rays to destroy cancer cells. The type of radiation used depends on the stage of the cancer. This treatment modality is usually reserved for those cases that cannot be treated surgically.
Chemotherapy, which uses drugs to destroy cancer cells, may be used to treat basal cell carcinoma. In most cases, the chemotherapy drugs are applied directly to the skin in a cream or a lotion.
Photodynamic therapyalso may be used to treat basal cell carcinoma. In this treatment, a drug that is activated by light (called a photosensitizer or a photosensitizing agent) is injected into a vein. This drug is absorbed by all cells in the body, but collects at a higher concentration and remains longer in cancer cells. One to three days after the injection, when most of the drug no longer remains in normal cells, a laser is focused on the lesion, activating the drug and destroying cancer cells.
An oral medicationis a recent option for treating basal cell carcinoma. In 2012, the U.S. Food and Drug Administration (FDA) approved vismodegib (Erivedge) to treat locally advanced and metastatic basal cell cancer in adults. This medication is administered in pill form and is taken once per day. It should not be used in women who are pregnant or who may be pregnant.
Prevention
As much as possible, avoid or minimize exposure to direct sunlight between 10 a.m. and 3 p.m.
Block the sun’s rays with protective clothing such as hats and long sleeves.
Before going outside, apply (and reapply often) a waterproof sunscreen lotion with a sun protection factor (SPF) of at least 30.(大多数人很少涂抹防晒霜,一个SPF of 30 really provides only about an SPF of 15.)
Avoid sunlamps and tanning booths.
Perform regular skin self-examinations, looking for any new growths, sores that don’t heal, or changes in the shape, color, or size of existing lesions.
People who have had one basal cell skin cancer have an approximately 50% chance of having a second nonmelanoma (basal or squamous cell) skin cancer within five years. For this reason, preventive measures are especially important after initial diagnosis.
Get annual checkups and make sure your skin gets a thorough going-over. Ask your doctor about any spots you're concerned about.
When To Call Your Doctor
Make an appointment with your doctor when you notice a new growth, particularly on sun-exposed sites. Just about everyone has some skin growths; most are harmless. Nonetheless, an examination is wise and a biopsy may be needed. A non-healing lesion or a growing lesion should be looked at promptly for early detection.
Schedule a skin examination at least once a year following an episode of basal cell skin cancer.
Reviewed by Kevin Berman, M.D., Ph.D., Atlanta Center for Dermatologic Disease, Atlanta, GA. Review provided by VeriMed Healthcare Network.