Let's Talk About Migraines
We've got the doctor-approved scoop on causes, symptoms, treatments, and a jillion other tips that make migraine life easier.
If you’re reading this, we guess you're on a first-name basis with the mega-headache monster known as migraine. Or maybe you’ve just been introduced and need to confirm. Or perhaps your concentration issues are actually caused by the monster's sneaky cousin: silent migraine. (Yep, it exists, and not just in fairy tales.) Whatever migraine answers you're looking for, we've got them. Here, top neurologists give you the lowdown on causes, symptoms, and the best headache-zapping treatments and lifestyle changes so you can get your life back with a lot less pain and strife.
Our Pro Panel
We went to some of the nation's top experts in migraines to bring you the most up-to-date information possible.

Marius Birlea, M.D.
Assistant Professor of Neurology; Director, Headache Fellowship
University of Colorado Denver School of Medicine
Denver

Joel R. Saper, M.D.
Director
Michigan Headache & Neurological Institute
Ann Arbor, MI

Stewart J. Tepper, M.D.
Professor of Neurology
Geisel School of Medicine, Dartmouth
Lebanon, NH
Typically anywhere between four and 72 hours. Those who have chronic migraines (more than 15 attacks a month) tend to have headaches that last longer (but still within that window).
Typically, you get a throbbing, pulsating pain on one side of your head, and you feel queasy. You might also be super-sensitive to bright lights or loud sounds. Some people get dizzy, too. One in five patients experiences an aura right before the headache part—either flashing lights, zigzags, or bright colors—or sometimes has trouble speaking or thinking of words. Sometimes the aura takes the form of obscured vision (like tunnel vision).
You can either prevent migraines from happening via drugs or devices that stimulate your brain, or you can take meds to stop an attack once it comes on. These medications range from pain relievers like Advil to newer drugs that target specific brain chemicals thought to be causing the pain.
Your genes basically. Most people with migraines have a parent who had them and that makes your brain more vulnerable to certain triggers, whether it’s stress or smells or your hormones. When something sets off an attack (say, sleeping in on Saturday or drinking a glass of wine), there's a reaction inside your brain that affects the parts responsible for feeling pain as well as processing light and sound.
What Are Migraines Anyway?
You’d be forgiven for thinking migraines are really horrible headaches. They can be, but you can have a migraine without much pain at all.
Instead, you might have troubling focusing at work or feel queasy or actually vomit. You might be particularly sensitive to light or find that you’re seeing zigzags.
And that’s because migraines are actually an inherited neurological disorder, and headache is just one of its symptoms. So-called regular headaches can cause a lot of pain, but they’re usually caused by a variety of external factors, from tension and hunger to blocked sinuses, neck pain, or (worst-case scenario) tumors.
Migraines can also sometimes be triggered by external stimuli, especially when they accumulate (so you slept badly, are having a stressful day, and you skip lunch, for instance). But people with migraines have a sensitive brain that reacts to these triggers in a particular way that’s still not entirely understood.
There are three regions in the brain that seem to play an important role in migraines—the hypothalamus, the part of the brain that regulates body temperature, sleep, and hormones, among other things—and the upper and lower brain stem.
During the time leading up to the migraine, these three areas of the brain start to change in the way they relate to one another:
The neural cells in these areas begin sending out messages via neurotransmitters, including serotonin and glutamate. These signals activate some areas of the brain, like the parts that control sensory information (such as light and pain), and suppress others (such as the areas that control concentration and attention).
In many people, this flood of serotonin and other neurotransmitters causes the release of a small protein-like molecule called calcitonin gene-related peptide (CGRP). When CGRP gets released, it leads to inflammation in the covering of the brain (called the meninges) as well as in the blood vessels, causing them to dilate. It’s that combination of inflammation and dilation that produces that throbbing pain.
The whole process can last anywhere from four to 72 hours.
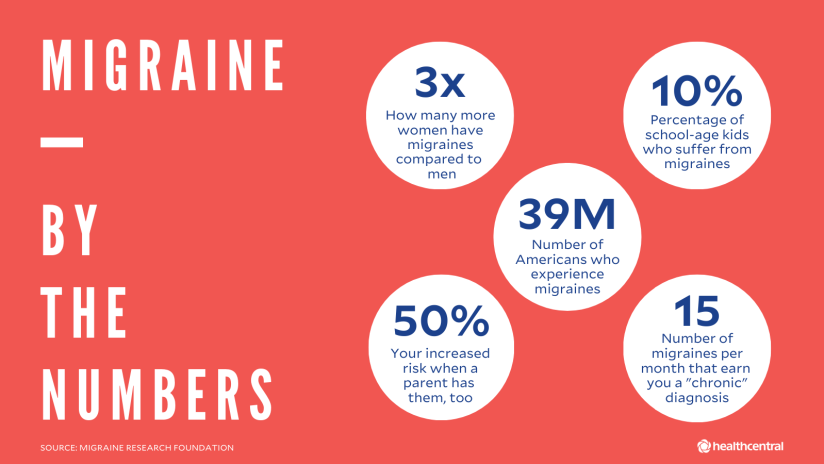
And this experience is not uncommon—migraines plague 39 million Americans, or one in four American households, according to the Migraine Research Foundation. Women are three times more likely to have migraines than men (18% versus 6%), but the 10% of school-age kids who suffer from them are evenly split between boys and girls. Most people who have them are between 18 and 44, and half had their first attack before they turned 12.
These brain attacks also derail your day. In fact, migraines are the sixth most debilitating condition in the world, responsible for lost productivity and healthcare costs that the Migraine Research Foundation estimates to be as high as $36 billion a year in the U.S. alone.
What Causes Migraines in the First Place?
Short answer: No one knows for sure. But there are some risk factors that make you more susceptible to migraines.
Genetics
Between 80% to 90% of people who get migraines typically had a parent (usually a mom) who had them, too. Doctors think you inherit the sensitivity in the brain that sets the stage for an attack when everything lines up. For instance, if you’re predisposed to migraines and you aren’t getting enough sleep, then that lack of sleep along with, say, flickering lights can bring on a migraine. That genetic link is pretty strong. If your mom or dad had migraines, you have a 50% chance of having them. Both parents? That risk factor jumps up to 75%.
Another sign of this genetic predisposition: Kids can suffer from migraines, with symptoms ranging from dizziness to stomach aches. And there’s even a theory that colicky babies are crying because they have migraines, not gas. In a study of 1,400 new parents, researchers from the University of California, San Francisco discovered that moms who had a history of migraines were 2.5 times more likely to have infants with colic.
Gender
More women have migraines than men and that may have something to do with the relationship between estrogen and serotonin. When the levels of estrogen drop quickly—as they do right before your period—it also affects serotonin and possibly other brain chemicals responsible for triggering a migraine. Going through perimenopause is another high-risk time because estrogen is fluctuating so wildly. Surprisingly enough, about three-quarters of pregnant women report that their migraines get better (especially after the first trimester) because of the relatively high and stable levels of estrogen. The same is true for breastfeeding, which also keeps your estrogen levels from falling too fast.
That drop in estrogen is a trigger, not a cause of migraines. About a third of women don’t get migraines during their period.
Serotonin levels:
Serotonin is a neurotransmitter, a chemical molecule that carries messages from one brain cell to another. People with migraines tend to have abnormal levels, which fluctuate during an attack, but what role serotonin plays in this condition isn’t exactly clear. It could be that serotonin activates the pain pathways in the brain, causing the release of CGRP, or it could simply help activate the parts of the brain most susceptible to an attack.
A head or brain injury:
A concussion or whiplash can cause migraines and so can strokes, lesions from multiple sclerosis, and infections. All of these can damage the brain so that neurons are firing sporadically or continuously in a pathological manner, generating the symptoms of a migraine.
What About Migraine Triggers?
All sorts of things can set off a migraine attack in people who are prone to them, but everyone’s triggers are different. To make things even more complicated, the very things that set you up for a migraine one day may not set it off the following week. That’s because it could be the accumulation of triggers that can push you over your personal threshold for migraines, not just any one thing.
Common triggers include:
stress
poor sleep (or too much sleep)
weather changes (like high humidity or changes in barometric pressure)
bright lights
motion sickness
fatigue
going too long between meals
certain foods, especially ones that have their own chemicals that can affect your nervous system or mimic brain chemicals, like red wine or caffeine
What Are the Types of Migraines?
Migraines are classified into three different types.
Episodic Migraines
People with this type have fewer than 15 attacks per month, each one lasting between four and 72 hours. These are the most common sorts of migraines, and roughly 90% of migraine sufferers have these less frequent attacks (though if you’re edging into to half-the-month territory, they’re hardly infrequent).
Every year, about 2.5% of migraine sufferers progress from episodic attacks to chronic ones, and one of the culprits for the progression is over-using pain meds, including aspirin and Tylenol.
Chronic Migraine
Those with chronic migraines (CM) have 15 or more attacks per month, and their migraines tend to be more severe and last longer than those with episodic ones (though still within the four to 72-hour window). About 8% of people with migraines have CM, and these patients tend to have more co-existing illnesses as well, including depression, anxiety, as well as high-blood pressure and heart disease.
Migraines With Aura
About 20% to 30% of those with migraines have auras, or neurological disturbances. These auras last anywhere from five to 60 minutes (though typically they last longer than five minutes) and occur before the headache strikes. They include:
numbness or tingling
trouble getting words out
flashing lights or colors
tunnel vision
seeing zigzags
Not everyone experiences auras in the same way—you might get tunnel vision while your dad saw flashing lights. And the type of aura you get may change over time too.
One other thing: Women who have auras have an increased risk of strokes—as much as five times as women without migraines with auras—particularly if you’re younger than 40. (After 40, other factors, like smoking and high blood pressure, increase your risk more.) While this sounds scary, your doctor will work with you to make sure your risk stays as low as possible.
Silent migraine—These are a subtype of migraines with auras, but without the headache pain. In other words, you have speech difficulties and see flashing lights, zigzags or other visual disturbances, but without the throbbing that typically follows the aura.
Do I Have Symptoms of Migraines?
Migraines are no joke—90% of migraine patients can’t go about their normal routine, more than 25% miss at least one day of work a month, and one in three need to lie down until the attack ends. The signs of a migraine include:
Moderate or severe pain that gets worse when you do any kind of physical activity
A throbbing or pulsating headache, usually on one side of the head for about 60% of migraine sufferers; about 15% of those always get the pain on the same side of their head
A sensitivity to noise or bright lights and sometimes to smell and touch
Nausea or vomiting
Vertigo
A stiff or painful neck, either before, during, or after an attack
Exhaustion (usually after the migraine has ended)
To review, aura symptoms include:
Changes to your vision—you either lose it gradually (like tunnel vision or dark, Swiss-cheese like holes) or you see things like flashing lights or bright spots
Feeling numb or weak on one side
Tingling in an arm or leg
Trouble speaking or getting your words out
Hearing noises

If you have an aura, the warning signs that a migraine is coming on can be strikingly similar to the type of stroke known as transient ischemic attack (TIA). But there is a difference. A TIA is over fairly quickly, while auras are longer (usually from 20 to 60 minutes). But if you’ve just had an aura for the first time that was either very short or longer than an hour and your vision was obscured, call your provider or go to an urgent care clinic to get it checked out sooner rather than later.
What About Migraine Symptoms in Children?
Kids who have migraines tend to have similar symptoms to adults, though their attacks don’t last as long as adults and they may not have headaches. The other signs include:
Stomach pain
Headaches
Dizziness
Nausea or vomiting
Sensitivity to smells, sounds, lights and touch (your child may want to retreat into a dark, quiet room, for instance)
Mood changes (your kid gets more irritable or moody for no apparent reason)
If your child is having bad headaches and you (or someone other family member) suffer from migraines, then make an appointment with a headache specialist if possible. The doctor will take a thorough medical history so try to keep a record of your child’s symptoms.
When Should I See a Doctor?
When migraines start to interfere with your daily activities or you’ve progressed from episodic migraines to more than 15 attacks per month, it’s time to get help. In the last couple of years, there are many treatments for both types of migraines and they can be life changing.
The trouble is that many people, especially those with chronic migraines, don’t get the help they need—one study found that fewer than 5% consulted with a doctor, got treated, and then followed through with treatments.
And while primary doctors can diagnose migraines, sometimes it makes more sense to go to a neurologist or even go to a dedicated headache doctor or center that can manage your care and treat all your symptoms. (You can find both at the Migraine Research Foundation.) The problem, though, is that there are only 500 headache specialists for the 39 million people seeking relief.
How Do Doctors Diagnose Migraines?
Migraines are a diagnosis of exclusion—your provider will have to rule out other causes before saying you have migraines. To do this, doctors will perform the following:
Take a Medical History
You’ll be asked to describe your headaches as your doctor asks you some questions, including:
Is your headache better when you lie down, or when you sit up?
Is your headache worse when you bend over, or when you strain for a bowel movement? Does your headache change on the weekends?
What makes your headache better and what makes them worse? And where does it hurt? Does it hurt anywhere else at other times?
Is it burning, or pounding, or throbbing?
When you have a headache, would you rather be in a sunny or dark room? What about a quiet room?
There’s also a set of criteria by the International Headache Society that doctors follow to make a diagnosis for migraines with or without auras. Patients must have two of the following four features when it comes to headache pain:
It must be moderately to severely intense
It tends to occur on one side
It has a throbbing or pulsating quality
It has to get worse with routine physical activity
And they have to have one of the following two criteria while they’re having an attack:
Not being able to tolerate light and noise
Nausea and/or vomiting
If you have auras, they must include:
Visual or sensory symptoms that only last as long as your migraine attack
They come on gradually
They’re usually followed by a headache, but not always. In fact, you may not have a headache (so you have a silent migraine) or you have such a mild one that the headache isn’t very apparent
Finally, a patient has had to have at least five attacks in their lifetime.
Imaging Tests
Not everyone needs a CT scan or MRI to rule out migraines. But to decide who does, doctors ask red-flag questions to see if there might be something more serious going on (like a brain bleed or underlying health condition, for instance). So a doctor will want to know if something happened before your headaches started.
They’ll likely ask if you’ve recently had an infection or a blow to the head. Or if your headaches started after the age of 50 and came upon you suddenly and very painfully (in the rare case you have an aneurysm that’s leaking blood). Or if the patterns to your headaches changed in any way—you now get them every day when you used to have them occasionally and they’re getting worse (a sign you might have a tumor).
What’s the Best Treatment for Migraines?
There are two types of treatment—the type that prevent attacks, or at least lower the number and intensity (known as preventative); and treatments that you take during an attack (known as acute). Even when you do take preventative medication, you usually have to have something on hand during an attack to decrease the pain. There are also complementary treatments that include lifestyle changes that help keep triggers at bay.
Since 2018, new migraine meds that target CGRP have come onto the market that have sharply reduced the number of headaches people have every month—by as much as 75% in about half these patients. But because not everyone can take drugs (think pregnant women or those trying to conceive) there are also non-drug devices that can prevent attacks or help during one.
Medication for Acute and Preventative Treatment
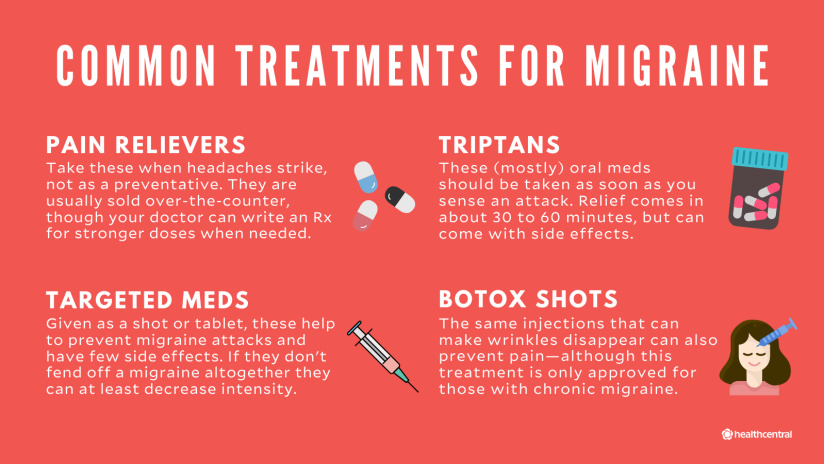
Pain relievers
These are used when headaches strike and are usually sold over-the-counter, though sometimes a doctor can write Rx for stronger doses. Some of the more common ones include:
Aleve (naproxen sodium)
Advil (ibuprofen)
Tylenol (acetaminophen)
Excedrin (which contains aspirin, acetaminophen, and caffeine)
It’s best not to take more than the recommended dose, nor should you rely on them if you have more than 10 attacks per month. Overusing even OTC pain relievers can cause rebound headaches in people with migraines—the medication itself triggers more headaches that follow the attack. These rebound headaches go away once you stop taking too many pain relievers.
Off-label Drugs
Sometimes doctors will prescribe drugs that are meant for other things in an effort to prevent headaches. These include:
Birth control pills, for women who have migraines before their periods unless they have migraines with auras. Those women have a higher risk of strokes, so doctors are reluctant to put them on hormonal contraception, which raise the risk even more—in fact, about seven times more than women who have migraines without auras and who are not on birth control.
Antidepressants, like Zoloft (sertraline) or Prozac (fluoxetine), in an effort to raise serotonin levels
Anti-seizure drugs, like Topamax (topiramate) that block excess glutamate, another neurotransmitter involved in migraines
Triptans
These (mostly) oral meds target serotonin receptors and are meant to be taken as soon as you feel a migraine coming on. They usually provide relief in about 30 to 60 minutes, though they can make your nausea worse.
These medications aren’t recommended during pregnancy, nor for people with high blood pressure, history of strokes, or those with Raynaud syndrome, because they can narrow the arteries. And you can overuse them too and make your migraines worse. Medications include:
Maxalt (rizatriptan)
Imitrex (sumatriptan), which also comes in a nasal spray
Meds That Target CGRP
These new drugs, some of which prevent attacks in the first place, come in the form of shots (either done in a doctor’s office or by you at home) or tablets. They block CGRP molecules or its receptors so the chemical doesn’t flood the brain during an attack.
The preventatives, most monthly injections, are designed to cut the number of migraine attacks and have few side effects, mostly pain at the injection site and constipation. And the preventatives can be so effective at decreasing the intensity of a migraine (as well as how often it happens) that you might just need an OTC pain reliever during an attack. They include:
Aimovig (erenumab)
Ajovy (fremanezumab)
Emgality (galcanezumab)
A new, once-daily oral medication that is also a preventative was approved by the FDA in late September 2021 and is due to launch in early October 2021. It is called:
Qulipta (atogepant)
Other oral meds are taken during an attack to relieve the pain. These include:
Ubrelvy (ubrogepant)
Nurtec (rimegepant)
All these CGRP-targeting medications are FDA-approved for both chronic and episodic migraines. But in order to get insurance to pay for them, you have to prove you have tried the older meds (like triptans) and they’ve failed.
Botox Shots
The same injections that can make wrinkles disappear can also prevent migraines, although they are only approved for people with chronic migraine and tend to work better for those who have many headaches a month. A doctor gives you several shots (sometimes as many as a dozen or more) around your head, neck, and shoulders, and the toxin blocks the pain receptors in those muscles and nerves, preventing them from sending signals to the brain.
There are some rare, but scary side effects (like drooping eyes) but the most common one is a headache after the injections (it goes away). Each set of injections last about 12 weeks, and you have to prove that you’ve tried other treatments without success.
Non-Drug Devices
If you don’t want to go the drug route, you can try a pulsating device that blocks migraine pain by sending electrical signals to the brain. These devices include:
The Cefaly device is an electrode attached to a strap (it looks a bit like a small heart-monitor) that you wear on your forehead. You can use it during an attack, leaving it on for an hour as it buzzes the nerves going into the brain. You can also use it every evening for 20 minutes to prevent pain.
The single-pulse transcranial magnetic stimulation device (sTMS) is about the size of a shoe and contains a magnet that pulses. You put it on the back of your head and the magnetic pulses stimulate electrical activity in the brain. You used to twice a day to prevent migraines, and give yourself four more pulses during an attack.
Nervio is a patch you wear on your arm that you activate during a migraine with a cellphone app. It sends signals to your brain stem to block the pain. It’s only approved for people with episodic migraines.
Complementary or Lifestyle Treatments
Along with medical treatments, you can also try improving things about your daily habits that may be setting you up for attacks, like insomnia or stress. Some of the more common lifestyle suggestions by doctors include:
Getting better sleep. People with migraines have trouble drifting off or staying asleep. They also tend to have sleep apnea and other sleep busters that leave them feeling unrefreshed when they wake up. So a doctor may work with you to get you on a sleep schedule (going to bed and waking up at the same time) and leaving your phone in another room so you’re not tempted to look at it if you wake up at 3 a.m.
Eating healthier. There is some evidence to show that obesity can turn episodic migraines into chronic ones. So try to eat more plant-based meals and swap out unhealthy foods like soda and sugary treats for more fruits and veggies.
Stress management. Meditation, mindfulness, yoga, biofeedback—all these are proven stress relievers. Yoga and tai chi in particular are mind-body exercises that can reduce the pain and frequency of migraine attacks, especially if you practice regularly.
What’s Life Like for People With Migraines?
For people who have episodic migraines, life is pretty normal between headaches. But since you can’t anticipate triggers and attacks, your life can also get unpredictable. Chronic migraines can be disabling emotionally and physically. Your productivity goes down and there’s a lot you cannot do. There are also a number of co-existing conditions that can occur when you have migraines, especially those with chronic migraines. These include:
Depression and anxiety. About 30% of chronic migraine patients and 17% of those with episodic migraines also have depression. But it’s still not clear whether there’s a link between depression and migraines because of serotonin levels or whether your quality of life thanks to migraines spurred the depression. People with episodic and chronic migraines also often have anxiety and panic attacks.
Ulcers and/or gastric bleeding. People with migraines are three times as likely to have these gastric conditions, partly because taking aspirin and NSAIDs can affect the gastric lining.
Insomnia and other sleep disorders. You’re eight times more likely to have a sleep disorder when you have migraines, though the connection isn’t clear. But sleeping badly can give you more headaches and make the pain worse—which in turn can make it harder to sleep.
Chronic pain conditions, including inflammatory arthritis.
High blood pressure, high cholesterol, and other cardiovascular disorders, especially those who have chronic migraines.
Where Can I Find My Migraine Community?
Top Migraine-Related Instagrammers
Amy, @the_migraine_life
Follow because: If you’ve looked up “migraine” on Instagram before, you’ve likely already stalked Amy’s feed. But if you’re new around here, Amy should be one of your first migraine follows. Since she started having headaches in 2015, she’s documented every step of the way, from her first neurologist appointment, to her pain and activity tracker, and everything she’s learned about this headache-of-a-world.
Danielle Newport Fancher, @migrainewriter
Follow because: She starts tough conversations about migraines that need to be had. In doing so, she raises awareness about the condition and gives you talking points for when you need to explain migraine to your friends, family, and even your doctors.
Natalie Sayre, @mindfulmigraine, mindfulmigraine.org
Follow because: Like you, she never thought she’d be here, hanging in this community of migraineurs—but now that she’s here she’s made it her mission to share every tip and tipping-point to living with migraine. She shares hacks (like blue-light glasses), and how to navigate relationships with migraine.
Mark Canadic, @migraineprofessional, migraineprofessional.com
Follow because: He deems himself the “health detective”—probably because, if there’s an alternative and holistic treatment for migraine, he’s going to hunt it down, try it, and tell you all about it. He believes in the connection between the brain, gut, and hormones, so his alternative treatments target the trifecta. The info makes for an interesting (and worthy!) follow but always be sure to check with your doc before going on your own alternative treatment journey.
Jaime Sanders, @migrainediva, themigrainediva.com
Follow because: Her migraines do not care if she’s homeschooling her son, doing a speaking engagement for a migraine org, or just trying to put on some make-up to feel “normal.” They hit her hard, and hang for days, sometimes weeks. Despite all that, she pushes through to be a mom and advocate—and that alone will push you along, too.
Top Migraine-Related Podcasts
Holistically Healing. Stacie Younger, a holistic health coach, had migraines that mimic strokes and anxiety that paralyzed her. She credits a holistic lifestyle where she eats as clean as possible for showing her migraines and anxiety the door—and she shares all about how she did that on her podcast.
The Migraine Miracle Moment. While this podcast is hosted by neurologist and migraine sufferer Dr. Josh Turknett, it is not heavy on the medical jargon. It simply talks about his experience with migraine, how he helps it with diet and lifestyle changes, and features others who have had success curbing their migraines with alternative treatments, too.
The Migraine Gut Podcast. Hosted by “The Migraine Guy,” Kevin Patton, this podcast breaks down the latest migraines news, treatments, and tips, and he even responds to listeners’ migraine questions.
Top Migraine-Related Orgs and Support Groups
It’s good to find organizations and groups that are all dedicated toward researching the causes of migraines and raising awareness about this condition. Even though there are millions of people just like you, many of them don’t get the help they need.
Association of Migraine Disorders. If you find yourself wanting to learn more (yes), get involved (you do), and wear cool shades (who doesn’t), then you’ll want to become a part of this community. They create fun campaigns (like #shadesformigraine) to help build awareness, and they provide tons of education for you and your family so you can beat migraine together.
Coalition for Headache and Migraine Patients (CHAMP). Their guides for overcoming insurance barriers, how to navigate COVID-19 with migraine, and resources for disability will make you feel empowered and even somewhat at ease. Their guidance is priceless.
American Migraine Foundation. Their “find a doctor” feature on their site is a draw in and of itself. Beyond that, their patient guides contain easy-to-digest information and they have endless ways of getting involved with your migraine community.
Migraine Strong. They’re a fierce group of women with varying degrees of migraine, who battle their conditions in a variety of different ways, and they welcome you, with open arms, into their support group. Tune in from afar by reading their stories and blog posts, or chime in to the conversation in their public Facebook group.
Migraine Research Foundation. Like the AMF, this non-profit provides a list of dedicated headache doctors as well as headache clinics.
Chronic Daily Headache and Migraine Support Group. This private Facebook group has about 28,000 members from around the world and is open to migraine and other chronic headache patients and those who love them who post about 80 times a day. It’s worth checking out if you want the support of people who know what you’re going through.
- Migraine Statistics (1): Migraine Research Foundation. (n.d.). “Migraine Facts.” migraineresearchfoundation.org/about-migraine/migraine-facts/
- Migraine Statistics (2): National Headache Foundation. (n.d.). “Statistics from the American Migraine Prevalence and Prevention Study.” headaches.org/2011/04/08/statistics-from-the-american-migraine-prevalence-and-prevention-study/
- Connection Between Colic and Migraines: Headache. (2019). “The Association Between Parental Migraine and Infant Colic: A Cross‐Sectional, Web‐Based, U.S. Survey Study.” headachejournal.onlinelibrary.wiley.com/doi/10.1111/head.13575
- Hormones and Migraines: Migraine Research Foundation. (n.d.). “The Impact of Hormones.” migraineresearchfoundation.org/about-migraine/migraine-in-women/the-impact-of-hormones/
- Breastfeeding and Migraines: American Migraine Foundation. (2017). “Migraine and Pregnancy.” americanmigrainefoundation.org/resource-library/understanding-migrainemigraine-and-pregnancy/
- Serotonin and Migraines: Cephalalgia. (2007). “Serotonin and Migraines: Biology and Clinical Implications.” ncbi.nlm.nih.gov/pubmed/17970989
- Differences Between Episodic and Chronic Migraines: Current Pain and Headache Report. (2012). “Defining the Differences Between Episodic and Chronic Migraines.” ncbi.nlm.nih.gov/pmc/articles/PMC3258393/
- Problems With Migraine Care: Headache. (2016). “Assessing Barriers to Chronic Migraine Consultation, Diagnosis, and Treatment: Results From the Chronic Migraine Epidemiology and Outcomes (CaMEO) Study.” ncbi.nlm.nih.gov/pubmed/27143127
- Migraine Symptoms: Practical Neurology. (2014). “The Clinical Features of Migraines With and Without Aura.” practicalneurology.com/articles/2014-apr/the-clinical-features-of-migraine-with-and-without-aura
- Migraine Treatments: Pain Treatment and Research. (2015). “Evidence-Based Treatment for Adults With Migraines.” ncbi.nlm.nih.gov/pmc/articles/PMC4709728/
- CGRP Preventative Medications: Abbvie News Center. (September 2021.) "FDA Approves QULIPTA™ (atogepant), the First and Only Oral CGRP Receptor Antagonist Specifically Developed for the Preventive Treatment of Migraine." https://news.abbvie.com/article_display.cfm?article_id=12338
- Migraines and Comorbidities: Journal of Headache and Pain. (2020). “Comorbid and co-occurring conditions in migraine and associated risk of increasing headache pain intensity and headache frequency: results of the migraine in America symptoms and treatment (MAST) study.” thejournalofheadacheandpain.biomedcentral.com/articles/10.1186/s10194-020-1084-y
What to Read Next

8 Things to Do Before (and After) a Migraine Attack

Can Therapy Help You Have Fewer Migraine Attacks?

Everything You Need to Know About Chronic Migraine Auras



